Total Shoulder Replacement
This brochure offers a brief overview of shoulder anatomy, arthritis and total shoulder arthroplasty. This information is for educational purposes only and is not intended to replace the expert guidance of your physician. Please direct any questions or concerns you may have to your doctor.
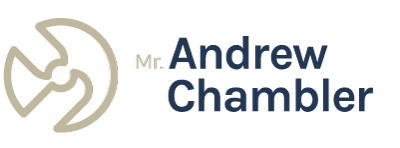
Shoulder anatomy
The shoulder joint is similar to a ball-and-socket joint that is comprised of three main bones: the collarbone (clavicle), the shoulder blade (scapula) and the upper arm bone (humerus), which extends from the shoulder blade to the elbow.
The upper end of the humerus where it rotates is a smooth, rounded head (ball) that fits into the glenoid cavity (socket) of the shoulder blade. Because the ball is larger than the socket, it is more flexible, but has less inherent stability. Muscles, tendons and connective tissue protect the shoulder joint and hold the various parts together.
Because the shoulder joint is stabilized by muscles and tendons, rather than by bone, the shoulder has great flexibility. This gives the shoulder joint a wide range of motion, enabling movements such as lifting, pushing and pulling. However, this great degree of motion has a trade-off; the stability of the shoulder is dependent upon the surrounding soft tissue and can result in a larger number of problems not faced by other joints supported by bony structures. A healthy shoulder can be damaged by disease or injury, resulting in severe pain, pseudoparalysis (false paralysis) and muscle weakness.
Shoulder Conditions
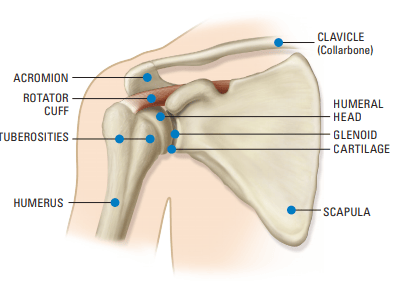
Osteoarthritis
Osteoarthritis (degenerative arthritis), the most common form of arthritis, affects nearly 21 million people in the United States. It is a condition that causes wear and tear to your joint cartilage and develops after years of constant motion and pressure on the joints. As the cartilage continues to wear, the joint becomes inflamed and can result in unbearable pain and decreased range of motion. If non-surgical treatment options such as medication, physical therapy or lifestyle changes fail to provide relief, your surgeon may recommend a surgical treatment, including shoulder replacement.
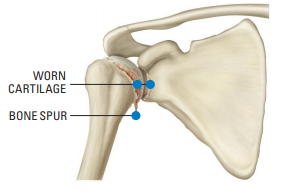
Inflammatory (Rheumatoid) Arthritis
Inflammatory arthritis is a chronic joint disease that can attack any or all joints in the body. It can strike at any age and affects more women than men. In the shoulder, inflammatory arthritis causes the synovium to thicken and form a tissue growth (pannus) that clings to the protective cartilage and releases chemicals that attack and destroy it. The joint may become
red and swollen, and pain may radiate into the neck and arm. Over time, the joint may become stiff and the muscles may weaken from lack of use. The bone also may be destroyed.
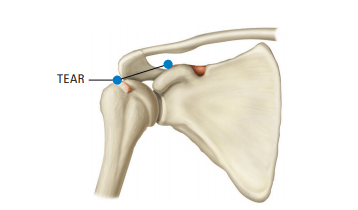
Rotator Cuff Tear
Most people with a small cuff tear can be treated arthroscopically. Surgery for rotator cuff tears usually occurs when a patient has a combination of shoulder arthritis and a massive irreparable rotator cuff tear. The rotator cuff is a group of muscles/tendons (supraspinatus,
infraspinatus, teres minor and subscapularis) that surround the shoulder in order to keep the shoulder centered while performing shoulder-related tasks such as elevating and rotating the upper arm.
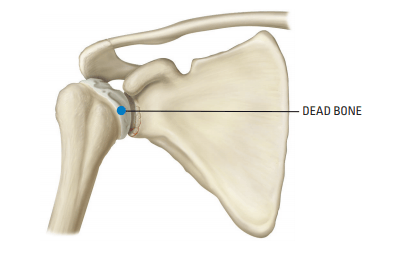
Avascular Necrosis
Avascular necrosis is a disease in which there is a temporary or permanentloss of blood supply to the bone. A number of conditions, including longterm use of steroids or alcohol, a traumatic injury, rheumatoid arthritis or unhealed fractures can cause the blood supply to the bone to be cut off. As the bone dies, it collapses. Although avascular necrosis can happen in any bone, it usually affects the ends of long bones such as the humerus.
When this happens, the shoulder becomes painful and movement becomes limited.
What are my treatment options?
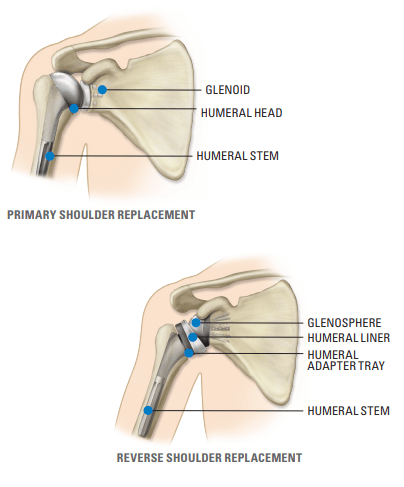
Shoulder replacement surgery replaces the damaged part of your shoulder. Sometimes, only the ball is replaced. Other times, both the ball and socket are replaced. The ball is usually metal and the socket is usually plastic. During surgery, an incision is made in the front of the shoulder. Once your surgeon exposes your shoulder joint, the surgeon will remove the damaged bone and cartilage. The head of the humerus is then removed so your humeral shaft can be prepared for the insertion of the metal stem and ball. In the case of a total shoulder arthroplasty, the socket (glenoid) portion of your shoulder will also be resurfaced and replaced to re-create the natural contours of the bones in a healthy shoulder. In cases where only the humeral head is replaced, a hemiarthroplasty is performed. Both are options for patients with painful and disabling shoulder joints
Shoulder replacement surgery is used for inflammatory arthritis sufferers to relieve severe arthritic pain and inflammation that does not respond to medication or physical therapy. Surgery can improve pain and mobility, and is typically done only after age 50 since artificial joints tend to wear down after 10 to 15 years.
Depending on the severity of the rotator cuff tear, your doctor may opt to perform a reverse shoulder replacement. In this procedure, the anatomy of the shoulder is reversed by attaching a metal ball to the shoulder bone and a plastic socket to the upper arm bone.
Your surgeon may recommend that you do not have surgery, but instead participate in supervised therapy. However, operative treatment is the most universal solution for these types of fractures that can be fixed. Depending on the age and severity of the fracture, your doctor may suggest a hemi (partial) or reverse shoulder replacement surgery. The procedure usually helps regain shoulder function and reduces the amount of pain.
The goal of treating avascular necrosis is to improve the use of the joint and to stop it from collapsing further. Treatment options will be based on your condition and may include medication, physical therapy or shoulder replacement surgery.
Total shoulder replacement
The shoulder is the third most frequently replaced joint after the hip and knee. Lack of range of motion and pain that affect day-to-day activities are the main reasons patients consider this operative treatment.
Primary vs. Reverse Shoulder
A primary shoulder replacement mimics the natural anatomy of the shoulder: a plastic “cup” is fitted into the shoulder socket (glenoid), and a metal “ball” is attached to the top of the upper arm bone (humerus). In a reverse total shoulder replacement, the socket and metal ball are switched.The metal ball is fixed to the socket and the plastic cup is fixed to the upper end of the humerus. A reverse total shoulder replacement typically works better for people with cuff tear arthropathy because it relies on different muscles to move the arm.
Surgery
Joint replacement surgery is a major operation. As with any major operation, there are possible complications. Some of these are related to anesthesia, while others are associated with the joint surgery itself. Every possible effort is made by the medical team to prevent complications, but this cannot be accomplished without your participation. Therefore, it is important that patients know about the following, which include but are not limited to, infection, blood clots, implant breakage, malalignment, stiffness, dislocation and nerve damage. Any of these can require additional surgery.
Although implant surgery is successful in most cases, some patients still experience stiffness and pain. No implant will last forever and factors such as a patient’s age and activity level can affect longevity. Your surgeon will discuss these and other relevant risks with you.
There are many things that your surgeon will do to minimize the potential for complications. Your surgeon may ask you to see your family physician before surgery to obtain tests
to better understand your medical condition.
After surgery you will receive pain medication and begin physical therapy. Depending on the procedure, you may be encouraged to use your arm soon after the surgery. You also may be asked to begin shoulder exercises to regain motion and strength. The specifics of your rehabilitation will be determined by your surgeon based on your condition.
Most patients are ready to go home between one to two days after surgery and may be asked to do shoulder exercises at home or with supervised therapy. You will be shown a variety of exercises designed to regain mobility and strength in your shoulder. It is important to follow the physical therapy protocol provided by your surgeon in order to facilitate the recovery process.
Exercise is crucial for proper rehabilitation. Therapy may begin the same day as your surgery and may continue up to four to six months post-op. Proper rehabilitation and willingness to follow all of your surgeon’s recommendations will contribute to a more successful recovery after surgery. Most patients are able to resume waist-level activities (writing) and possibly driving three to four weeks post-op depending on your surgeon and your condition. Activities such as golf, tennis and swimming can usually be resumed, but only after a thorough evaluation by your surgeon. Recovery time will vary for each patient.
High-impact activities or contact sports are typically not recommended. These types of activities place an extreme amount of pressure on the joints, which could lead to complications. Your surgeon will discuss this with you. Your surgeon will likely continue to evaluate your progress during the life of the prosthesis on a yearly basis. These evaluations may or may not require X-rays. It is important to see your surgeon if you notice any unusual changes regarding your new joint.
Summary
This information is not intended to replace the experience and counsel of your orthopaedic surgeon. Surgery is one of the most important decisions you will make. Shoulder replacement has allowed millions of people to live with less pain and to return to more active lifestyles.
Your surgeon will help you decide if it’s the right choice for you. With any surgery, there are potential risks, and results will vary depending on the patient. Joint replacement surgery is not for everyone. Check with your physician to determine if you are a candidate for joint replacement surgery. Your physician will consider the risks and benefits associated with this procedure, as well as individual factors such as the cause of your condition, and your age, height, weight and activity level.